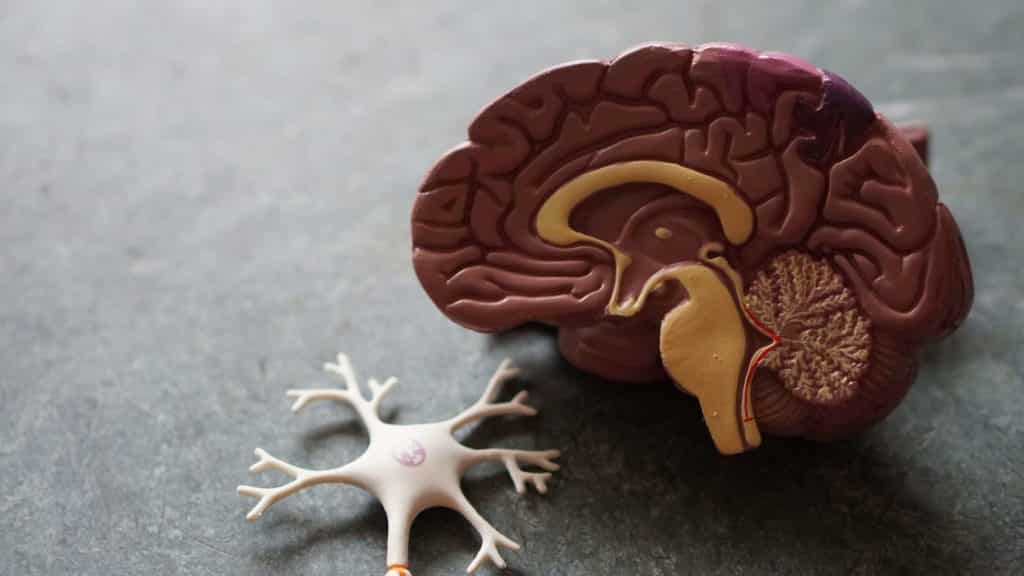
Chiari malformations are caused by a malfunction in the cerebellum (the brain region that governs balance) that causes part of the cerebellum to be placed below, rather than above, the entrance of the spinal canal. If this happens, the cerebellum and brain stem may be forced into the skull and surrounding the spinal canal’s opening (foramen magnum), causing tremendous pressure and a blockage of the cerebrospinal fluid. There are four forms of Chiari malformation based on brain tissue morphology and the presence of developing brain/spine abnormalities.
- Type I Chiari malformation (most common). Patients with type 1 don’t usually show symptoms until late childhood or adulthood since the brain and skull are still maturing. Patients with different Chiari malformations are often identified while still in the womb, at birth, or in early childhood.
- Type II Chiari malformation. Below the foramen magnum, both the brainstem and the cerebellum are involved. Spina bifida and myelomeningocele, a sac-like hole in the back where the spinal cord is exposed to the air, are often connected with this disorder. This condition affects youngsters and is also known as Arnold Chiari malformation.
- Type III of the Chiari malformation. The most dangerous kind is Type III, which is quite rare. The cerebellum and brainstem generate a pouch-like structure that protrudes from the back of the head and neck, holding brain tissue. Chiari III is a condition that causes severe neurological problems.
- Type IV of the Chiari malformation. This kind of Chiari malformation, also exceedingly rare, comprises an incomplete or underdeveloped cerebellum.
What causes Chiari malformation?
The most frequent kind of Chiari malformation is “congenital” or “primary” Chiari malformation. This kind of CM is caused by structural problems in the central nervous system that develops in the womb, potentially resulting from a genetic mutation or a shortage of nutrition during pregnancy. Secondary CM, often known as “acquired” CM, develops later in life due to significant cerebrospinal fluid loss caused by infection, illness, or severe injury.
One or more of the following factors contribute to the symptoms of a Chiari malformation:
- Compression of the cranial nerves
- Compression of the brainstem
- Compression of the cerebellum
- Normal cerebrospinal fluid (CSF) flow is disrupted.
- Increased pressure in the CSF
- Damage to the nerves
- Chiari symptoms may be exacerbated by coexisting illnesses such as syringomyelia, intracranial hypertension, or other hereditary abnormalities.
What Symptoms Does a Chiari Malformation Have?
The Chiari type I malformation is most often diagnosed in adults, with symptoms such as:
- Coughing, sneezing, or straining may cause headaches.
- Neck ache
- Injury to the spinal cord (myelopathy)
- Cerebellar symptoms include involuntary eye movements, speech pattern disturbances, and muscular control loss (especially in the trunk)
- Speech issues, swallowing difficulty, involuntary eye movements (particularly gazing down), hoarseness, palate weakness, tongue atrophy, recurrent aspiration, and sleep-related breathing disorders such as sleep apnea are indications of the lower brainstem.
- Vision issues with things that seem to leap or vibrate, hearing loss, sluggish heart rate, lightheadedness/fainting, hiccups, weakness, muscular spasms, hyperactive reflexes, and Babinski reactions are some of the less frequent symptoms.
- Symptoms of the central spinal cord include hand weakness, dissociated sensory loss, and loss of feeling in the shoulders and back (cape anesthesia)
The Chiari II malformation is most often identified in newborns and young children, and the following symptoms may occur:
- Difficulties swallowing/feeding
- Wheezing/stridor
- Breathing has stopped (apnea)
- A feeble scream
- Eye motions that aren’t voluntary
- Extreme sluggishness
- Despite significant abnormalities, some Chiari II individuals have average IQ and are self-sufficient.
The mortality rate for Chiari type III is substantial. Those who survive the newborn phase may have the following symptoms:
- Neurological deficits that be severe
- Mental deficiency
- Epilepsy
- Muscle spasms or low muscle tone
- Signs of upper and lower motor neurons
- Palsies of the lower cranial nerves
Because patients do not survive, data on symptoms are scarce. Chiari type IV abnormalities are often incompatible with life.
Chiari Malformation Diagnosis
The advancement and availability of magnetic resonance imaging (MRI) have shown that Chiari malformation is not as uncommon as previously believed. This complicated and dangerous neurological illness manifests itself in a variety of ways. The majority of individuals experience various symptoms, although others have none. Because each situation is unique, a skilled neurosurgeon is required for diagnosis.
Because patients with Chiari malformation type I are generally asymptomatic, the disorder may be discovered during a routine physical examination for another reason. A combination of patient history, neurological examination, and magnetic resonance imaging is used to make the diagnosis (MRI). To confirm a diagnosis, three-dimensional CT imaging or specific MRI scans known as CINE investigations may be employed.
Infants with Chiari type II may have difficulties swallowing, irritability, drooling, gagging or vomiting, limb weakness, neck stiffness, and developmental delays.
Once a Chiari malformation has been identified, it should be assessed by a neurosurgeon who specializes in the condition. Early identification and treatment are critical, and surgical outcomes for Chiari malformation type I are most significant when the problem is addressed quickly. After surgery, many patients continue to have considerable symptom alleviation and can resume normal activities without limitation.
Treatment for Chiari Malformation
Chiari malformation has no cure, although therapy may assist in alleviating symptoms and improving quality of life. Treatment for Chiari type I is determined by various criteria, including the severity of symptoms and the presence of a syrinx. When a patient has no signs of neurological abnormalities, a neurosurgeon will usually treat the problem by keeping a close eye on them. Pain-relieving drugs may be used when symptoms are modest but controllable.
Surgery may be required if a patient develops symptom progression, neurological impairments, or an increasing syrinx. When surgery is necessary, an incision is typically made in the center of the back of the head and continues halfway down the back of the neck. The muscles near the base of the skull and on the rear of the first cervical vertebra are gradually separated.
After separating the muscles, a craniectomy is done to expand the aperture at the base of the skull and provide extra room for CSF flow adjacent to the brain. A little piece of bone approximately the size of a silver dollar is meticulously shaved using a specialized surgical tool. After that, the first cervical vertebra is removed carefully by a laminectomy technique. In certain circumstances, further cervical lower lamina excision may be required.
What Are the Consequences of a Chiari Malformation?
The risks of concussion and post-concussion syndrome are enhanced in people with Chiari type I malformation.
In some instances, Chiari malformation progresses and might result in additional issues, such as:
- Spina bifida (spina bifida) (incomplete closing of the spine and spinal cord covering)
- Cystic fibrosis (a cyst or cavity forms in the spinal cord)
- Hydradenosis (buildup of excess fluid within the brain)
- Syndrome of the tangled line (tissues attach to the spinal cord, causing limited movement of the spinal cord within the spinal column)